Optimal contrast enhancement is important for a succesful diagnostic CT-scan.
In this article we will discuss:
The purpose of contrast-enhanced CT (CECT) is to find pathology by enhancing the contrast between a lesion and the normal surrounding structures.
Sometimes a lesion will be hypovascular compared to the normal tissue and in some cases a lesion will be hypervascular to the surrounding tissue in a certain phase of enhancement.
So it is important to know in which phase a CT should be performed depending on the pathology that you are looking for.
Scroll through the images to see the enhancement in the different phases.
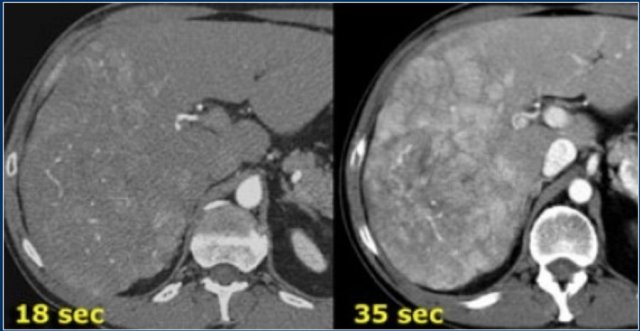
Hypervascular lesion is best seen in late arterial phase.
Timing of CT-series is important in order to grab the right moment of maximal contrast differences between a lesion and the normal parenchyma.
The CT-images show an early arterial phase in comparison to a late arterial phase.
The CT-images are of a patient who underwent two phases of arterial imaging at 18 and 35 seconds.
In the early arterial phase we nicely see the arteries, but we only see some irregular enhancement within the liver.
In the late arterial phase we can clearly identify multiple tumor masses.
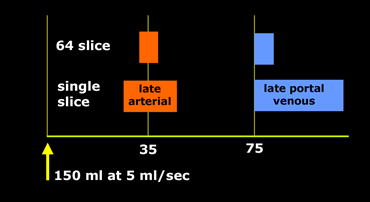
You have to adapt your protocol to the type of scanner, the speed of contrast injection and to the kind of patient that you are examining.
If you have a single slice scanner, it will take about 20 seconds to scan the liver.
For late arterial phase imaging 35 sec is the optimal time, so you start at about 25 seconds and end at about 45 seconds.
However if you have a 64-slice scanner, you will be able to examine the whole liver in 4 seconds. So you start scanning at about 33 seconds, which is much later.
In aterial phase imaging the time window is narrow, since you have only limited time before the surrounding liver will start to enhance and obscure a hypervascular lesion.
For Late portal venous phase imaging it is different. Here you don't want to be too early, because you want to load the liver with contrast and it takes time for contrast to get from the portal vein into the liver parenchyma. Besides you have more time, because the delayed or equilibrium phase starts at about 3-4 minutes.
So you start at 75 seconds with whatever scanner you have.
In many protocols a standard dose is given related to the weight of the patient:
In some protocols we always want to give the maximum dose of 150cc, like when you are looking for a pancreatic carcinoma or liver metastases.
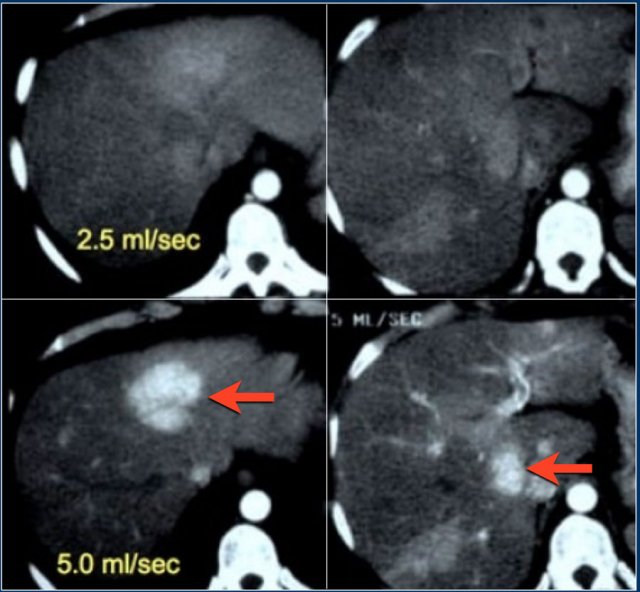
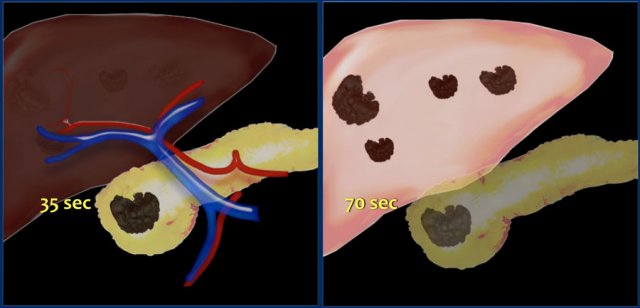
Patient with liver cirrhosis and multifocal HCC injected at 2.5ml/sec (left) and at 5ml/sec (right)
5cc/sec through a 18 gauge i.v. catheter
3-4cc/sec through a 20 gauge pink venflon
The upper images are of a patient with liver cirrhosis and multifocal hepatocellular carcinoma examined after contrast injection at 2.5ml/sec.
Because of poor enhancement the examination was repeated at 5ml/sec.
There is far better contrast enhancement and better tumor detection.
Some prefer to give positive oral contrast to mark the bowel.
This however has some disadvantages:
We use fat containing milk as negative oral contrast or if the patient doesn't drink milk we simply use water.
Polyethylene glycol (PEG) is also used, and Volumen®, which is a low density barium suspension.
PEG and Volumen® have the advantage that there is better bowel distension.
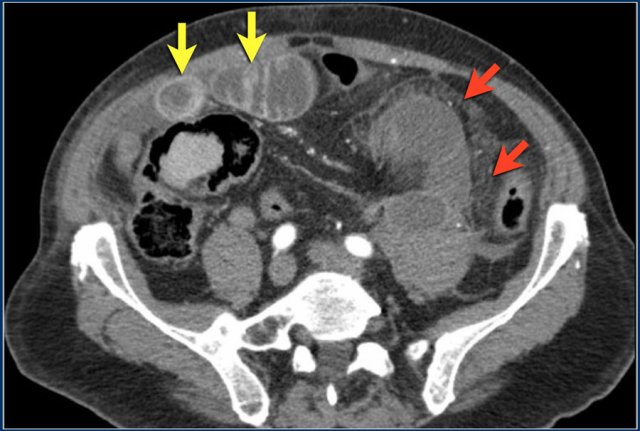
The CT-image shows nice enhancement of the normal bowel wall (yellow arrows) and no enhancement of the infarcted bowel (red arrows).
This would not be visible if positive oral contrast was given.
Rectal contrast is given in cases of suspected bowel perforation or anastomosis leakage.
We use positive contrast: 750 cc water with 50 cc non-ionic water soluable contrast.
More information is given in the protocol anastomosis leakage.
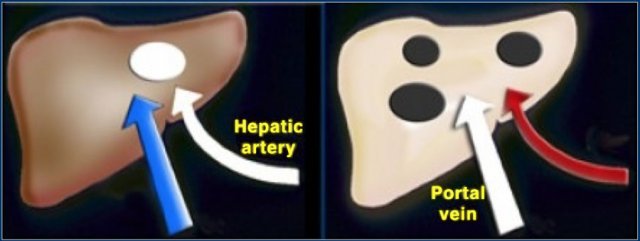
Hypervascular tumor (left) enhances in late arterial phase. Hypovascular tumor (right) enhances poorly and is best seen in the hepatic phase
The conspicuity of a liver lesion depends on the attenuation difference between the lesion and the normal liver.
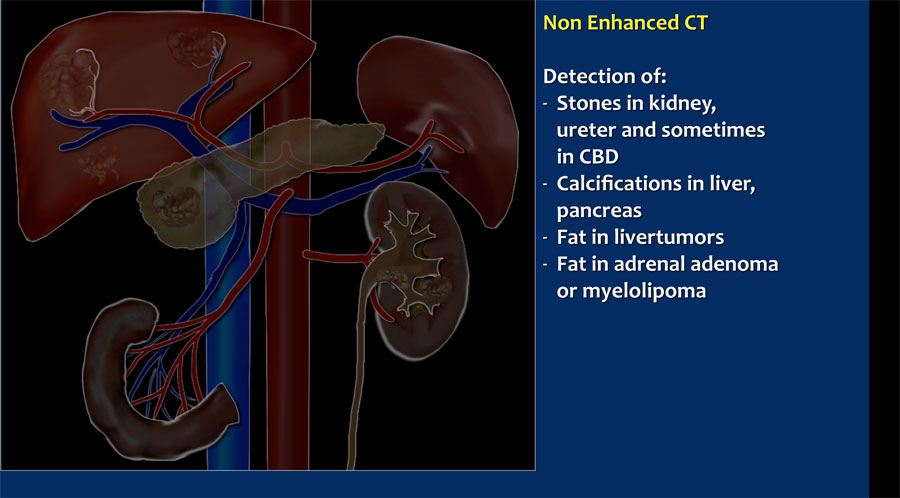
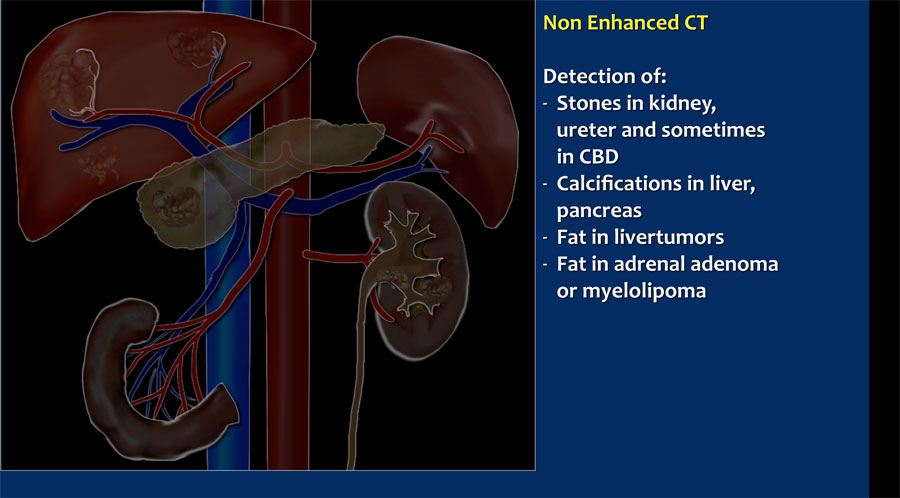
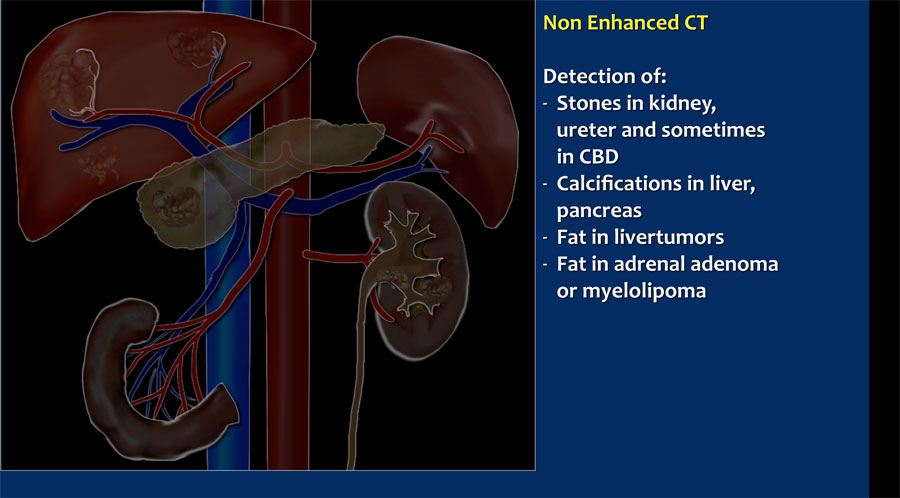
On a non enhanced CT-scan (NECT) liver tumors are not visible, because the inherent contrast between tumor tissue and the surrounding liver parenchyma is too low.
When we give i.v. contrast, it is important to understand, that there is a dual blood supply to the liver.
Normal parenchyma is supplied for 80% by the portal vein and only for 20% by the hepatic artery, so the normal parenchyma will enhance maximally in the hepatic phase at 70-80 sec p.i. and only a little bit in the late arterial phase at 35-40 sec p.i..
All liver tumors however get 100% of their blood supply from the hepatic artery.
So a hypervascular tumor will be best seen in the late arterial phase.
A hypovascular liver tumor however will enhance poorly in the late arterial phase, because it is hypovascular and the surrounding liver does also enhance poorly in that phase.
This tumor is best seen when the surrounding tissue enhances, i.e. in the late portal (or hepatic) phase at 75-80 sec p.i.
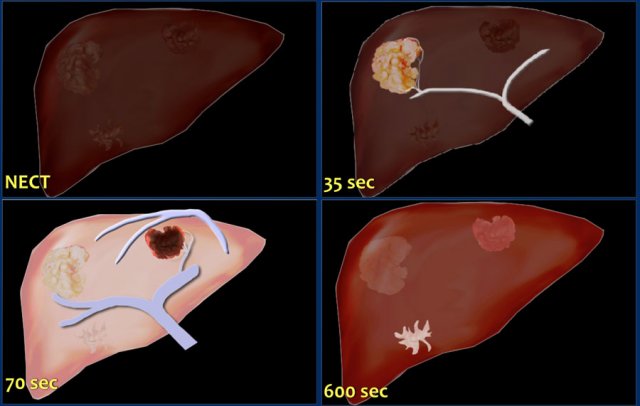
This figure is to summarize the enhancement patterns.
In the late arterial phase at 35 sec hypervascular lesions like HCC, FNH, adenoma and hemangioma wil enhance optimally, while the normal parenchyma shows only minimal enhancement.
Hypovascular lesions like metastases, cysts and abscesses will not enhance and are best seen in the hepatic phase at 70 sec p.i.
Fibrotic lesions like cholangiocarcinoma and fibrotic metastases hold the contrast much longer than normal parenchyma.
They are best seen in the delayed phase at 600 sec p.i.
This late enhancement is comparable to what is seen in cardiac infarcts in MRI of the heart.

If you want to characterize a liver lesion, you need maximum contrast at a maximum flow rate, i.e. 150cc contrast at 5cc/sec. through a 18 gauge green venflon.
In most cases you also want to scan the whole abdomen.
You can do this either at 35 sec or 70 sec p.i.
We do not routinely perform a NECT in order keep the radiation dose as low as possible.
When you know in advance, that you are dealing with hypovascular metastases, a hepathic phase at 70 sec p.i. is sufficient.
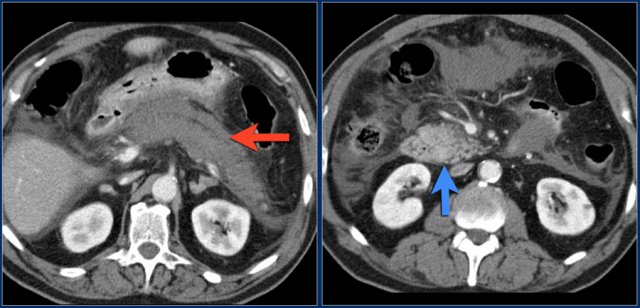
Pancreatic carcinoma is best imaged at 35 sec p.i. Liver metastases are best imaged at 70 sec p.i.
Pancreatic carcinoma is a hypovascular tumor and is best detected in the late arterial phase at 35-40 sec p.i. when the normal glandular tissue enhances optimally and the hypovascular tumor does not.
Metastases in the liver are best detected at 70-80 sec p.i., when the liver parenchyma enhances optimally.
In some cases it can be difficult to differentiate a pancreatic carcinoma from a focal chronic pancreatitis.
A NECT can be included in the protocol to detect calcifications in the pancreas, but we do not use that in our standard protocol.
Some radiologists use a longer delay for scanning of the pancreas at 50 sec p.i.
Imaging in acute pancreatitis is best done after 72 hours of presentation. read more.
Ct performed in the first two days can underestimate the severity of the disease.
Necrosis can be best detected in the late arterial phase at 35 sec p.i.

CT examination of the pancreas should always be done with maximum amount of contrast at a maximum flow rate, because both small pancreatic carcinomas aswell as pancreatic necrosis in pancreatitis are difficult to detect.
It is a matter of personal flavor to do the whole abdomen at 35 sec p.i. or at 70 sec p.i.
Some perform one single CT somewhere inbetween 35 and 70 sec, but that is not what we prefer.

Especially in small bowel obstruction (SBO) you need to answer the most important question: is there strangulation?
To answer that question, you need a contrast enhanced CT for the following reasons:
Do not use positive oral contrast, because this will obscure bowel wall enhancement.
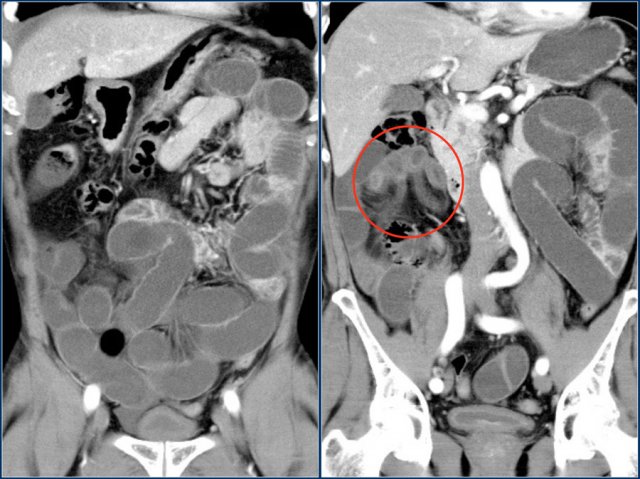
The coronal reconstruction nicely shows bowel wall enhancement in a patient with ileus due to a small bowel obstruction.
Notice the cluster of thick walled loops with poor enhancement and edema of the mesentery (red circle).
This is a closed loop obstruction with strangulation. This patient needs immediate surgery.
If this patient would have been given positive oral contrast, you probably would not have notice the ischemic bowel.
Leakage after bowel surgery is a great clinical problem.
Patients, who are suspected of leakage, need the best CT-protocol they can get and you as a radiologist need the best images to convince the clinician.
You do not want to tell the surgeon that there is probably leakage, but you are not sure.
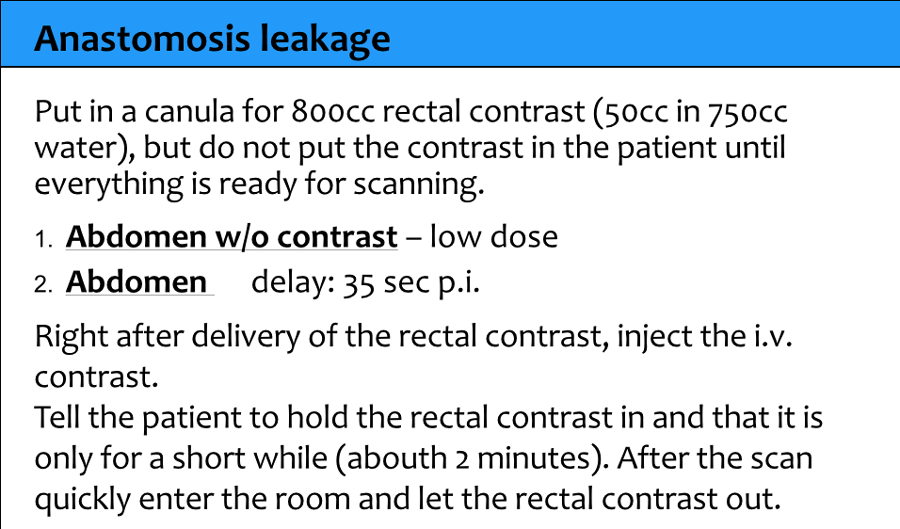
A NECT without any oral or rectal contrast is needed to compare with the CECT with rectal contrast, because you don't want to end up in a discussion whether some hyperdense stuff outside the bowel is leakage or some post-operative material, dense bowel content or contrast from an earlier examination.
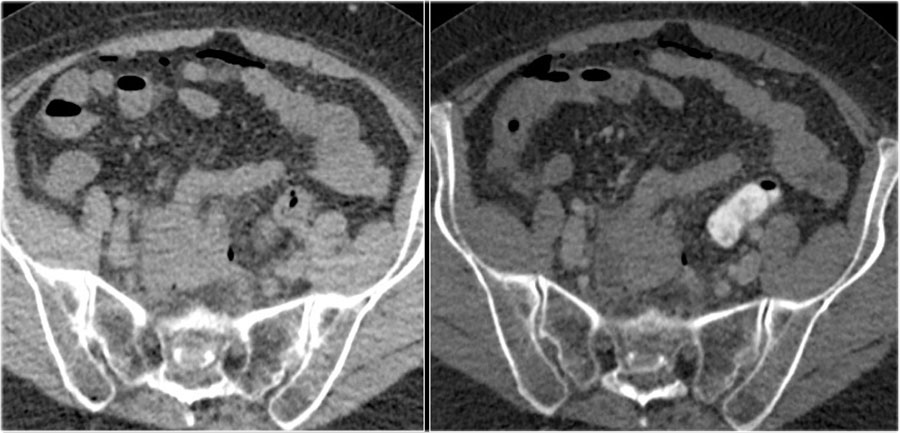
Anastomotic leak. Images on the left prior to rectal contrast and on the right after rectal contrast.
Anastomotic leak. Images on the left prior to rectal contrast and on the right after rectal contrast.
Here a patient with an anastomosis in the lower abdomen after resection of a sigmoid carcinoma.
Compare the NECT without oral or rectal contrast on the left with the images on the right after rectal contrast.
There is no doubt, that contrast in the fluid collection in the right lower abdomen is the result of leakage from the bowel (arrow).
Good quality CT scanning is the most important factor for the diagnosis of pulmonary emboli.
On a poor quality scan it is impossible to rule out emboli.
We prefer to scan from bottom to top, because if a patient can't hold his breath, then you will have less breathing artefacts in the lower lobes, where most of the emboli are located.
In the upper lobes breathing does not cause that much movement as in the lower parts of the lung.
We ask the patient to breath in normally and hold his breath to avoid the transient interruption of contrast, which will be explained in a moment.
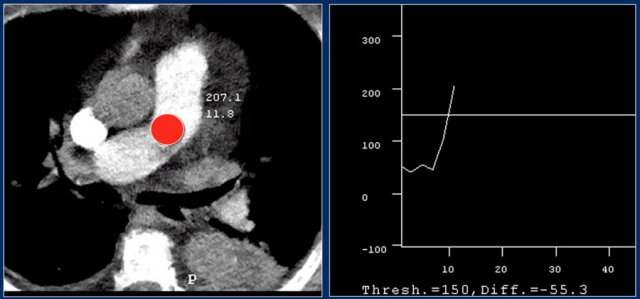
For good timing bolus tracking is needed.
A ROI is placed in the pulmonary trunk.
When the treshhold of 150 HU is reached, the patient is asked to breath in and scanning is started immediately.
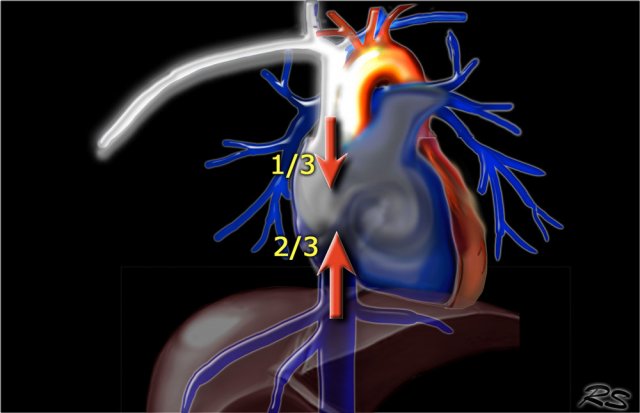
Transient Interruption of Contrast: Deep inspiration results in dilution of contrast in the right atrium by unopacified blood from the inferior vena cava.
TIC is a flow artefact, that consists of relatively poor contrast enhancement in the pulmonary arteries, while there is good enhancement in the SVC and also in the aorta, which seems not logic at all.
This vascular phenomenon occurs when the patient performs a deep inspiration just before the scan starts, resulting in increased venous return of unopacified blood from the inferior vena cava (IVC).
More unopacified blood from the IVC than opacified blood from the SVC enters the right atrium resulting in poor enhancement of the pulmonary arteries.
This phenomanon is especially seen in younger patients, who are capable of deep inspiration.
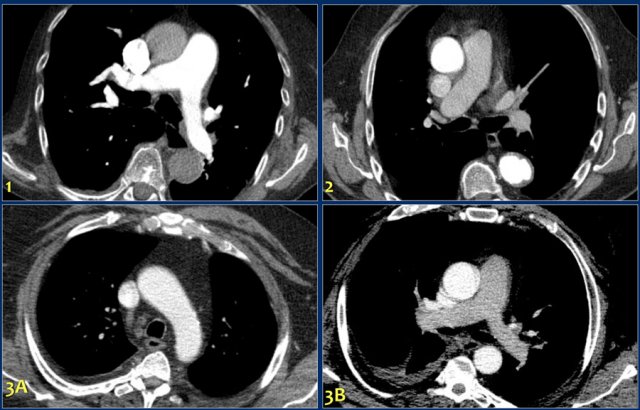
1. Optimal 2. Too late. 3. Transient interruption of contrast
The quality of CT depends on good contrast delivery and perfect timing.
Scans for pulmonary emboli are frequently of poor quality in young patients and of good quality in old patients.
The explanation is the following:
The images demonstrate: